The Science of Dry and Dehydrated Skin, by Dr. Anjali Mahto
This blog contribution by Dr. Mahto is geared to cosmetic formulators. Disclaimer - the content is a bit more advanced. Whether you’re developing products, work as an estheticican or are a regular consumer keen to learn more about the science of dry skin, this post will take you through a deep dive into the topic. Thank you Anjali for contributing to The Eco Well blog! Stay tuned! From here on out, we will be regularly featuring educational posts from scientists in and around the cosmetics space. Our goal is to create a knowledge-sharing platform, accessible to anyone :).
Skin is considered to be the largest organ of the human body accounting for 12 to 15% of body weight and covering 1.5 to 2 square metres of area. It is a highly dynamic and complex organ with a large number of specific roles. Aside from providing a key physical barrier to the outside world, it is also the site of significant endocrine, immunological and metabolic function. The skin forms part of the vital communication network between the inside and outside world. But even this is only half the story. The skin is not only an indispensable biological organ, but one could argue it functions as a social organ as well. It plays an important cosmetic role having potential impact on one’s social interactions, confidence, body-image, job prospects and even mate selection. Skin is often rightly or wrongly also used crudely as a surrogate marker for the perception of an individual’s general health status.
To be able to develop and formulate personal care products to supplement the skin and its numerous processes, it is important to have a solid understanding of the skin’s structure and function in both health and compromised or pathological states. The aims of this essay are to discuss basic skin physiology, maintenance of skin barrier health, and how this can be achieved. There will be a focus on how the skin behaves in a dry or dehydrated state and the impact of chemical agents that may drive this. Finally, strategies such as moisturisers and their selection will be reviewed as a method of breaking the dry-skin cycle and enhancing skin barrier function.
Source: BC Open Textbooks
1) Skin Structure and Function
The skin has three main layers each with its own primary function:
The epidermis which suffers as a barrier preventing loss of fluid and electrolytes as well as offering protection against external insult or injury
The dermis which is the source of structural and nutritional support
The hypodermis or subcutaneous fat layer which offers insulation
Whilst skin structure under light microscopy is fairly consistent in most body regions, there are well-recognised modifications in specialized areas such as the palms, soles, genitalia and scalp. Skin thickness can vary across sites with the epidermis of the eyelid measuring 0.06mm in contrast with the palms at 0.8mm.
1a) The Epidermis
The epidermis is the outermost layer of skin and its main cell type are known as keratinocytes, which account for 90-95% of cells. They are key in forming a physical, biological and chemical barrier to the outside world offering thermal protection as well as keeping out pollution, microbes and allergens.
The epidermis is arranged in stratified layers to include the basal layer (stratum basale), spinous layer (stratum spinosum), granular layer (stratum granulosum) and finally the stratum corneum. In certain areas where the skin is thick (e.g. acral sites such as the palms and soles), there is an additional layer known as the stratum lucidum which sits between the granular layer and stratum spinosum.
In contrast to the other layers, the stratum corneum consists of anucleated cells called corneocytes, which are derived from keratinocytes. Cells from the basal layer migrate and differentiate upwards until they form the stratum corneum. Dead cells are sloughed from the surface in a process known as desquamation. Under normal conditions, it takes two weeks for differentiating cells to leave the nucleated compartment and a further two weeks to move through the layers of the stratum corneum. The skin will therefore renew itself every 28 days.
The other main cells of the epidermis include melanocytes, Langerhans cells and Merkel cells. Melanocytes are the pigment producing cells of the skin. There is approximately one melanocyte to 36-40 keratinocytes. They are found in the basal layer of the skin where they make pigment granules known as melanosomes which contain melanin. These are transferred via dendritic processes to keratinocytes where they usually aggregate above the cell’s nucleus. Melanin is responsible for skin colour in addition to playing a major role in protecting the skin from ultraviolet radiation.
Langerhans cells are the third major resident cell type of the epidermis and play an important role in immune surveillance. They metabolize complex antigenic substances into peptides and once activated, migrate out of the epidermis into regional lymph nodes, functioning as antigen-presenting cells involved in immunity. The final group of cells are the Merkel cells which act as mechanoreceptors responsible for light touch sensation.
Source: Alsaab, Hashem. (2015). Thesis: Evaluation of the Percutaneous Absorption of Chlorpromazine Hydrochloride from PLO Gels Across Porcine Ear and Human Abdominal Skin. 10.13140/RG.2.2.11799.78248.
1b) The Dermis
Beneath the epidermis is a specialized structure known as the basement membrane, which attaches it to the next major layer, the dermis. The dermis is highly vascularized providing both structural and nutritional support to the skin. Its main cell type is the fibroblast which synthesizes collagen and elastin. The dermis can sometimes be further classified into the papillary (upper) and reticular (lower) dermis. The papillary dermis is rich in nerve fibres for detection of temperature, pain and itch sensation. The reticular dermis contains a densely packed matrix of collagen and elastin fibres alongside a glycosaminoglycan gel. These act together to give the skin strength, elasticity, and firmness. Blood vessels in the dermis play a key role in transport of nutrients and removal of waste products in addition to thermoregulation. A rise in body temperature triggers the dilation of blood vessels in the skin allowing heat to be lost from the surface; the opposite occurs in cold weather.
In addition to contributing to the skin’s tensile strength, the dermis is the site of key adnexal structures such as the hair follicles, sebaceous glands, apocrine and eccrine glands. These specialized tissues play their unique roles in the skin. Hair follicles are found all over the body except for the acral sites. When the weather is cold or strong emotion such as fear can trigger contraction of the arrector pili muscles which can cause hair in the follicle to stand up on end. Sebaceous glands are also attached to hair follicles and collectively a hair follicle, its arrector pili muscle and associated sebaceous gland are known as the pilosebaceous unit. Sebaceous glands produce sebum under the control of androgen hormones (e.g. testosterone, dyhydrotestosterone) to act as a lubricant for skin. Eccrine sweat glands can be found all over the body but occur in highest density in the axillae, forehead and acral sites. They aid temperature regulation; when the body needs to lose heat it will product sweat which will evaporate from the skin surface causing cooling. Sweat also functions to excrete organic toxins and heavy metals. Lastly, the apocrine glands found primarily in the axillae and anogenital region secrete a viscous, milky, odourless fluid previously thought to provide pheromone-like activity.
1c) The Hypodermis
The subcutaneous layer of skin consists primarily of adipocytes. It functions to absorb shock thereby offering mechanical protection in addition to insulating heat. Its thickness can vary depending on body site.
1d) Summary of Function
As demonstrated thus far, the skin clearly has a number of important functions to play aided by its unique structure and its resident cell types.
2) Understanding Dry Skin
Maintaining a healthy skin barrier is largely dependent on the process of desquamation in the epidermis. It will take approximately 28 days for a keratinocyte to migrate and differentiate from the basal layer and eventually be shed from the stratum corneum. Keratinocytes in the basal layer are the only viable cells of the epidermis. As they travel upwards, they start to lose the ability to undergo mitosis. As keratinocytes differentiate into spinous layer cells their shape becomes more polyhedral. Individual cells are held together by proteins known as desmosomes which require calcium-dependent enzymes for their formation. As the cells migrate into the granular layer, they contain keratohyalin granules which consist of proteins (e.g. profilaggrin, loricrin, involucrin, envoplakin) which will eventually form the cornified envelope of the stratum corneum. The cells finally move into the stratum corneum losing their nucleus, organelles and plasma membrane. Desmosome attachments become weaker and the cells are ultimately sloughed away from the surface. Skin disease can occur when this process is disrupted. Decreased shedding of skin cells from the surface will result in ichthyosis; increased epidermal cell turnover results in psoriasis. Impaired barrier function can be seen in Darier disease as a result of mutations in the ATP-dependent calcium pump in the epidermis.
Dry skin
One of the main functions of the epidermis is to prevent water loss and maintain hydration of the skin. Alterations in the barrier can result in increased water loss (known as trans-epidermal water loss, TEWL) and dry skin. Cosmetically dry skin has been noted to have a weaker barrier quality than normal skin. Disrupted desquamation can lead to lower cohesivity of skin cells. Dry skin has been shown to contain lower natural moisturising factors. Impaired barrier function will also facilitate the absorption of products being applied to the skin surface resulting in irritant contact dermatitis. Dry skin on a macroscopic level can appear rough, uneven, flaky, and even cracked or fissured. Symptomatically the skin may feel dry, tight, uncomfortable, painful or itchy. Individual or environmental factors may also work together to produce dryness. Underlying skin disorders (e.g. atopic dermatitis) and increased age as well as low humidity and temperature, exposure to solvents and some surfactants may contribute to dryness.
Source: skinetrate
Prolonged use of soaps and surfactants can have a negative impact on the skin barrier. They can emulsify lipids and denature proteins found in the skin resulting in increased TEWL and affecting the permeability barrier. Anionic surfactants tend to be the most problematic (e.g. C10-C12 alkyl chains, alkyl sulphates) in contrast to amphoteric surfactants which have a better safety profile. In addition to altering the water and skin surface chemistry, irritants may also potentially alter the natural microbial flora of the skin. Certain bacteria have been linked to higher rates of growth in alkaline pH and may have the ability to displace the normal skin microbiome.
3) The Stratum Corneum and Methods for Studying Barrier Function
Despite consisting of non-viable cells, the stratum corneum plays some key functions. Not only is it responsible for skin hydration, it functions as a mechanical and permeability barrier, in addition to keeping out reactive oxygen species from the environment, UV from sunlight as well as microbes. The stratum corneum is 12-16 layers thick. Its overall structure is of a “bricks and mortar” configuration where the corneocytes form the bricks, and the mortar is composed of intercellular lipids. The interaction between the two is responsible for the stratum corneum to function effectively as a physical and moisture barrier. The very outer layer of the stratum corneum has a slightly acidic pH of 4.5 to 6.5 (sometimes known as the acid mantle) due to sebaceous and sweat gland secretion. The acidic pH has antimicrobial properties. Corneocytes are flat and hexagonal in structure and packed in layers. They contain the protein, keratin, which binds water in addition to a second protein known as filaggrin on their surface. They have a cornified envelope rather than a plasma membrane and are connected to each other via corneodesmosomes.
Natural moisturising factors and intercellular lipids (ceramides, cholesterol and free fatty acids in a ratio of 3:1:1) are arranged in bilayers surrounding the corneocytes. They are formed in the granular layer of the skin and their hydrophobic properties prevent water loss into the environment. Moisture is maintained in the stratum corneum by the maintenance of natural moisturisation factors and desquamation. Moisture is also important in controlling rate of desquamation. In dry conditions, desmosomes remain intact resulting in a build-up of corneocytes and thickening of the stratum corneum. This will visibly be apparent as scaly skin. There are a number of methods by which stratum corneum barrier function can be measured. These can be classified into physical, instrumental and biological. Physical methods include tape stripping or stripping of the stratum corneum using cyanoacrylate glue. These can quantify the cells removed and light microsopy can visualize the cells directly. This method can be useful to assess the efficacy of a mosturising treatment from baseline. Instrumental methods include measuring TEWL through an evaporimeter. Skin hydration can be measured using Corneometer or SkinChip technology. Other methods for measuring epidermal thickness include confocal microscopy. In the research setting, MRI can be helpful on providing information on the internal structures of the epidermis and observing improvements with treatment. Biological methods to look at ultrastructural details of the stratum corneum and intercellular spaces utilize transmission electron microscopy, field emission scanning electron microscopy and immunofluorescence confocal laser scanning microscopy.
4) Product Formulation Strategies for Dry Skin
Moisturisers are an important part of daily skin care and their main goal is to maintain skin integrity and improve appearance by retaining water content, prevent TEWL and assist the skin’s natural barrier repair mechanism. Clinical signs of dry skin (xerosis) will appear when the water content of the stratum corneum falls below 10%. There are many options when choosing the components of a moisturiser formulation. Not only does the product need to support natural skin desquamation and maintain a healthy barrier, it also needs to reach a high aesthetic standard acceptable for consumer use. The basic components will usually consist of moisturising agents, water, emulsifier and preservatives. Most day moisturisers will be comprised of oil in water emulsions which are light and spread easily.
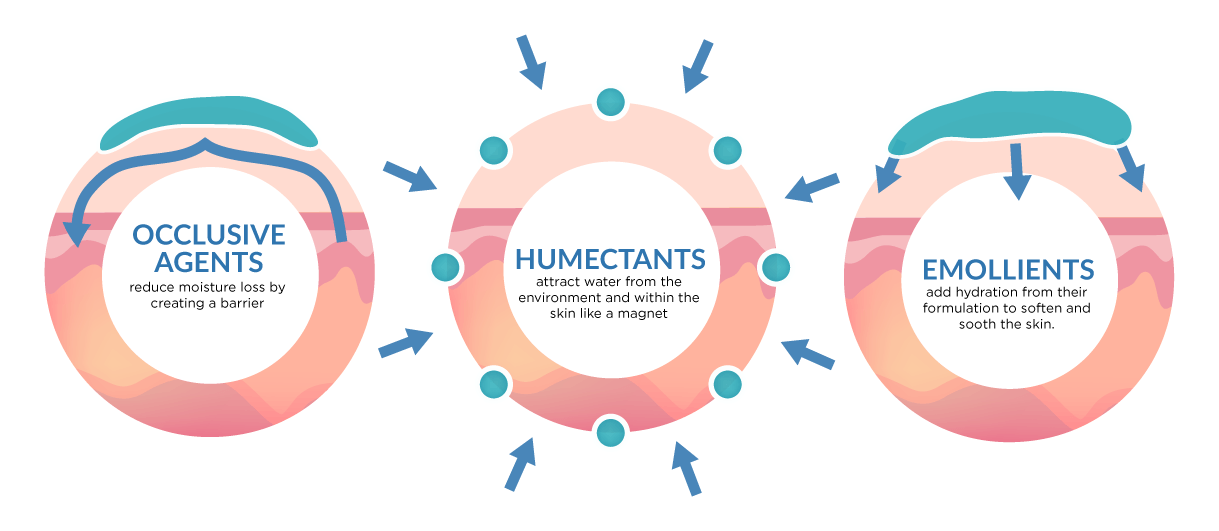
There are three main classes of moisturising ingredients: occlusives, humectants and emollients. A well-designed moisturising product for damaged or dehydrated skin will contain a combination of these classes of ingredient for best outcome.
Occlusive agents prevent TEWL by forming a hydrophobic barrier or film over the skin surface. This reduces evaporation from the statum corneum. Common examples include petrolatum, lanolin and beeswax. Petrolatum is highly effective but has an unfavourable, “greasy” texture. Lanolin use is generally limited due to its odour and allergenicity.
Humectants attract water from the viable epidermis and dermis (and also the environment if humidity is above 80%). This functions to increase corneocyte water content and promote normal desquamation. Glycerin, sorbitol, urea and sodium lactate are all examples of topically applied humectants. Glycerin, in particular, is one of the most commonly used compounds in cosmetic formulations and can be used in a range of different product types ranging from sticks, micro-emulsions and creams.
The third and final class is the emollients which work by filling in the gaps or spaces between the corneocytes and thereby smoothening the appearance of rough skin. They are usually lipids or oils which will repel polar water molecules and limit their passage to the outer environment. Depending on their inherent properties they can be further classified into protective, fatting, astringent or dry sub-types.
Source: VivaBuff
A good moisturiser may also contain special additives such as hydroxy acids, UV filters, vitamins, essential fatty acids and botanical agents depending on the desired end result. Thought must also be given to how active ingredients are delivered to the stratum corneum e.g cylodextrins and liposomes. Fragrance may be added to mask the odour of other ingredients or to improve the overall aesthetic quality of the product. Preservatives are essential to inhibit microbial growth and prevent lipids in the formulation becoming rancid. Moisturisers will also require an appropriate emulsifier system to create cosmetically elegant products. Non-ionic emulsifiers are usually the most common type used in skin care products. These include compounds such as alkoxylated alcohols, fatty acid ethoxylates, and glycol esters. Creating compounds with a balance of the above components will result in a moisturiser that will help restore water content as well as improve skin barrier function in skin which has become damaged or dehydrated.
5) Helping the Consumer Choose a Moisturiser
There is no doubt the product market is heavily saturated and helping the consumer pick the right moisturiser for their skin needs is vital. Descriptor terms such as the following may help:
Reduce dryness
Improve dull appearance
Smooth and soften skin
Increase firmness or suppleness
Immediate comfort
Long-lasting effect
Nourishing
Non-greasy
The challenge remains for a cosmetic formulator to deliver a product which is effective, causing minimal irritancy or allergenicity, with a minimal presence and pleasant aesthetic or sensory qualities.
Summary
The skin is a highly dynamic organ and not simply an inert brick wall despite the analogy we so often hear about its “bricks and mortar” structure. Keratinocyes undergo many changes as they migrate and differentiate from the basal layer to the stratum corneum where they are ultimately shed. The stratum corneum permeability barrier is composed of the cellular protein matrix as well as the intercellular lipids arranged in a bilayer. Both components are integral to maintaining desquamation, epidermal hydration and overall skin barrier function.
Moisturisers can be a useful way of managing damaged or dehydrated skin. If they are well-formulated they can reduce the impact of both internal and external factors (e.g. prolonged use of harsh surfactants) on stratum corneum permeability. They will also aid the self-repair mechanism of the skin by ensuring water content remains at a level that normal enzymatic function for dequamation can continue. Special additive ingredients can be used to fine-tune products for specific skincare concerns. Guiding the consumer when the product is ready to market by appropriate terminology can help make individuals make informed choices about product selection. Choosing the right product for the right concern will ultimately enhance the benefit of the treatment.
References
Loden M. Do moisturisers work? Journal of Cosmetic Dermatology, 2, 141-149
Lee T, Friedman A. Skin barrier health: Regulation and repair of the stratum corneum and the role of over-the-counter skincare. J Drugs Dermatol 2016; 15(9): 1047-1051.
Rawlings AV, Harding CR. Moisturisation and skin barrier function. Dermatol Ther 2004; 17 Suppl 1: 43-48.
Y Appa. Facial Moisturisers, in Cosmetic Dermatology - Products and Procedures, Draelos Z, ed. Blackwell Publishing, UK (2016) pp 132-137.
S Pillai, M Manco, C Oresajo. Epidermal Barrier in Cosmetic Dermatology – Products and Procedures, Draelos Z, ed. Blackwell Publishing (2016) pp 3 – 11.
J Del Rosso. Moisturiser and Barrier Repair Formulations in Cosmeceuticals, Draelos Z ed. Elsevier Canada (2016) pp 81-89.
G Grove, J Damia, T Houser, C Zerweck, Evaluating Cosmeceutical Efficacy in Cosmeceuticals, Draelos Z ed. Elsevier Canada (2016) pp 21-25.
T Vandergriff, Anatomy and Physiology in Dermatology, Bolognia J ed. Elsevier Ltd (2018) pp 44-55.
Written by Dr Anjali Mahto
Dr Anjali Mahto is a London trained consultant dermatologist and author of The Skincare Bible. She is spokesperson for the UK’s largest skin charity, the British Skin Foundation, and an executive committee member of the British Cosmetic Dermatology Group. Her work bridges the gap between traditional medical dermatology, beauty and cosmetic medicine. Her mission is to make trusted and reliable skin information accessible alongside improving science literacy and responsible influencing.
Find Anjali on Instagram @anjalimahto